The annual enrollment period for 2023 is right around the corner, which means HR professionals and management will be inundated with questions about any changes that are being made or changes employees would like to make to their plans. If you haven’t done so already, you may want to begin implementing a strategy for fielding questions and getting essential benefits information to employees.
At ProLiant, we’re benefits administration experts, and we’ve seen how bumpy the annual enrollment period can get, so we’ve put together some essential tips and information to help make the process a bit smoother. You can also reach out to us to learn about how ProLiant can simplify every annual enrollment period with ensured compliance and accurate reporting.
Implement a Communication Strategy for Annual Enrollment
The first step is to notify employees about open enrollment and to communicate any changes with employees as soon as possible. This includes providing the Summary of Benefits and Coverage (SBC) documents no later than the first day of open enrollment.
A good communication strategy will include various forms of communication, especially if your workforce is remote. Sending an email with the SBC documents is a good start, but consider utilizing other means of connecting so that you encourage conversation, questions, and action from your employees.
Here are some ways you can communicate with employees and ensure they are getting the information they need:
- Hold a company-wide webinar over Zoom to summarize benefit offerings and address frequently asked questions.
- Have team leads hold a Google Hangout meeting with their members and a benefits broker.
- Send a message to a special Slack channel so that everyone can share their questions and get answers.
Provide Essential Information to Employees About Their Benefits
Give plenty of information about plans and encourage questions throughout open enrollment. Encourage employees to look over their benefits elections again to ensure they don’t need to make any changes.
Remind employees that elections they make will remain in place for an entire year until the next enrollment period unless they experience a life-changing event, and if they don’t make new elections, they will have the same ones in place for the next year.
A lot can change for an individual in a year, so make sure employees consider what they may need to prepare for in the year to come. Employees may need to review the selections they’ve made in the previous year to ensure their benefits elections still fit in with their current budget and future plans.
Important aspects employees may want to consider further include:
There are many different concerns regarding benefits elections, but highlighting a few of these common points of interest in your communication strategy may encourage employees to take an active role in updating their elections. You may also consider using a benefits administration tool that streamlines the process and provides information to employees all in one place.
Many employees are looking for resources to address stress and mental health in the workplace, so be sure to provide any specific information on how they can access any tools your organization will make available to them in the next year.
Provide Employee Access to Provider Information and Resources
Make sure employees have access to representatives who can answer questions directly from your provider. Alternatively, your benefits broker may have documents and tools to help guide employees and address any frequently asked questions. Either way, these experts will be able to provide detailed insight and guidance for employees.
Stay Up-to-Date on the Affordable Care Act
Businesses with 50+ full-time employees must offer coverage to at least 95% of their full-time employees. If your business has fewer than 50 employees, it is exempt from the mandate. However, employers that are exempt and still wish to offer health coverage must meet certain ACA specifications.
You can learn more about the ACA Provisions for Employers and determine the size of your business on the IRS website or speak with a ProLiant expert today to see how we can simplify the entire process for your business.
What are forms 1094-C and 1095-C?
Form 1094-C: This form only goes to the IRS and provides a summary to the IRS about the employer, including number of employees, demographic information about the employer, and the number of 1095-C forms being sent.
Form 1095-C: This form goes to employees and the IRS and provides information about health insurance, including what coverage is offered to employees, the lowest-cost premium available, and when the coverage was available throughout the year. Employers with 50 or more employees must provide a 1095-C to all employees that are eligible for health coverage.
The information reported on these forms determines whether or not an employer is liable for payment under the employer shared responsibility provisions and the amount of payment. Form 1095-C is also used in determining the eligibility of an employee for the premium tax credit and to verify enrollment in minimum essential coverage for employees and their families.
You can learn more about these forms on the IRS website.
Provide Information About the ACA Open Enrollment Period for Individuals
If you have employees that will need to enroll for individual insurance via the Health Insurance Marketplace, you guide them to essential information from HealthCare.gov. Employees that will be enrolling in coverage for 2023 via the ACA can do so starting November 1st, 2022. In some situations, you can enroll outside open enrollment:
- Special Enrollment Period: Due to certain life events, you can enroll during this limited timeframe.
- Medicaid or CHIP: Those applying for Medicaid or CHIP can do so at any time, and coverage usually starts on the first day of the month you applied.
Visit HealthCare.gov to learn more about special situations.
Benefits Administration with ProLiant Makes Annual Enrollment a Breeze
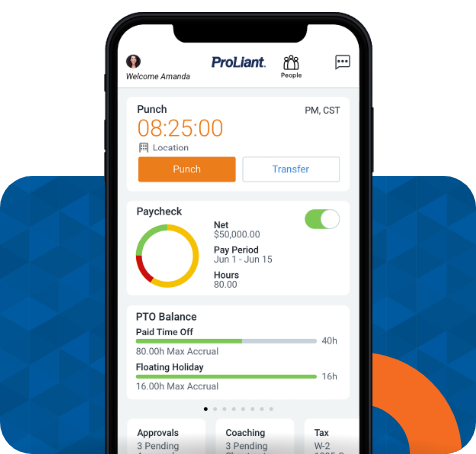
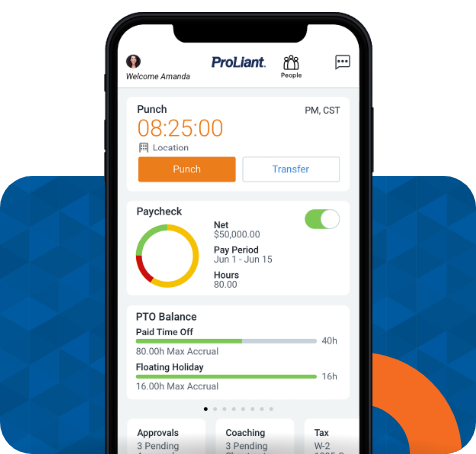
ProLiant’s Benefits Administration solutions streamline your employee benefits processes and ensure your employees are well informed about their options so that they can confidently make benefit enrollment decisions.
Here are a few ways we can make benefits administration easier for your business:
- Secure Data Sharing: Send your enrollment data to multiple insurance carriers seamlessly, securely, and accurately.
- Centralized Data: Centralize benefits data by securely archiving all HR and employee documents in a single location.
- Activity Reports and Insights: Compile and view a variety of activity reports for insight into employee data.
- Enrollment Alerts: Alert employees to complete enrollment and monitoring their status.
- ACA Assistance: We generate and file 1094-C and 1095-C ACA forms for you and provide ACA expertise.
If you’re interested in learning more about how we can help make annual enrollment easier for your business every year, request a meeting with one of our experts today.


No Comments Yet
Let us know what you think